When your kidney function has decreased to around 15%, dialysis will be necessary in order to survive. As your kidney function declines, your body will fill with extra water, salt and waste products. This condition is called uremia. Your hands or feet may swell. You will feel tired and weak because your body needs clean blood to function properly. Hemodialysis removes waste products and extra fluid from the blood by using a special filter called an artificial kidney, or a dialyzer. In-center hemodialysis is the most widely used method for treating kidney failure in the United States.
When your kidney function has decreased to around 15%, dialysis will be necessary in order to survive. As your kidney function declines, your body will fill with extra water, salt and waste products. This condition is called uremia. Your hands or feet may swell. You will feel tired and weak because your body needs clean blood to function properly. Hemodialysis removes waste products and extra fluid from the blood by using a special filter called an artificial kidney, or a dialyzer. In-center hemodialysis is the most widely used method for treating kidney failure in the United States.
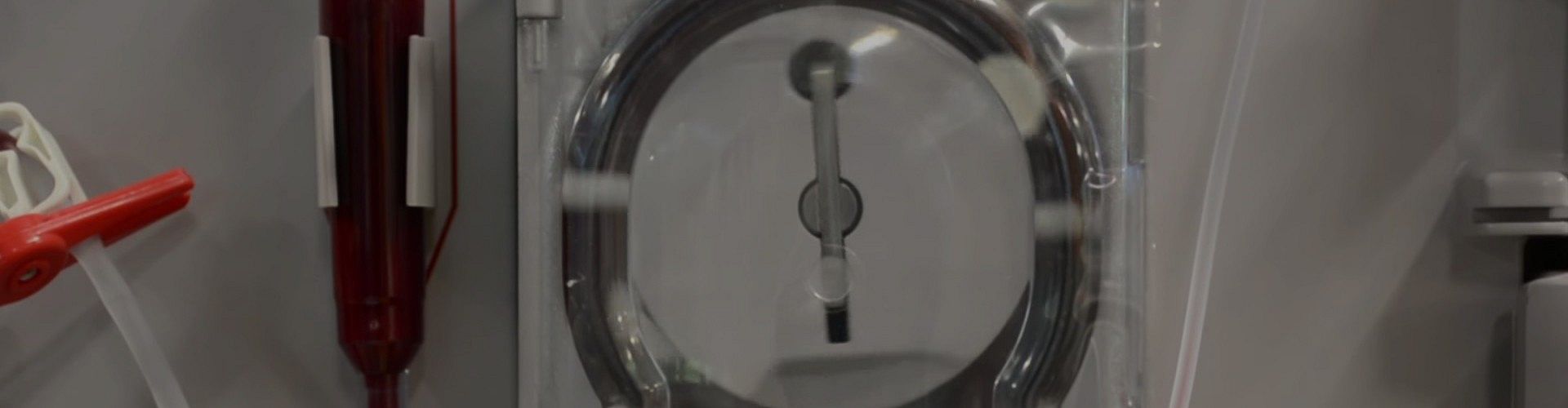
The dialyzer has two compartments. They are the blood compartment and the dialysate fluid compartment. The dialysate fluid is the fluid that cleans your blood. Your blood enters the dialyzer from the top and flows inside of the membranes. The membranes have tiny holes (pores) that are only big enough to remove the waste products and toxins. The important parts of your blood, like your red blood cells and protein, stay inside the membrane and are returned to your body along with your clean blood. At the same time your blood is entering the dialyzer from the top, the clean dialysate fluid enters the dialyzer from the bottom, surrounding each membrane that contains your blood. The blood and dialysate fluid move in opposite directions and do not mix. The dialysate fluid removes the wastes from your blood as it travels upward and outside of the membrane. When the dialysate fluid with the wastes reaches the top of the dialyzer (artificial kidney), the wastes and excess fluid leave the dialyzer and are sent to the drain. This is a continuous process.
In order to perform any type of hemodialysis treatment, a vascular access is required so there is a convenient entryway into your bloodstream. Placement of a vascular access requires a minor surgical procedure. Further discussion regarding vascular access is discussed in the “Peritoneal and Vascular Access Options,” chapter. When your vascular access is healed, it is used for the hemodialysis treatment by placing two needles into the access. The needles are attached to special tubing. The blood pump on the dialysis machine is set to move your blood from the first needle, through the tubing, and to the artificial kidney to be cleaned as described above. Your clean blood is then returned back to your body though the second needle. Only about a cup of your blood is outside of your body at any one time.
In-center Hemodialysis
 In-center hemodialysis is performed at a dialysis facility. Most dialysis facilities are set up as an open floor plan with recliners next to the dialysis machines. Hemodialysis treatments are usually performed three times a week. Each treatment lasts about four hours or as prescribed by your physician for your individual needs. Typically your dialysis treatment will require you to be weighed before and after each treatment to make sure the extra fluid is removed during dialysis. Specially trained nurses and dialysis technicians insert the needles and complete the treatment for you. Nurses and technicians are always there with you to monitor your blood pressure and your treatment. Routine lab tests will be scheduled and completed on your treatment day.
In-center hemodialysis is performed at a dialysis facility. Most dialysis facilities are set up as an open floor plan with recliners next to the dialysis machines. Hemodialysis treatments are usually performed three times a week. Each treatment lasts about four hours or as prescribed by your physician for your individual needs. Typically your dialysis treatment will require you to be weighed before and after each treatment to make sure the extra fluid is removed during dialysis. Specially trained nurses and dialysis technicians insert the needles and complete the treatment for you. Nurses and technicians are always there with you to monitor your blood pressure and your treatment. Routine lab tests will be scheduled and completed on your treatment day.
 Some clinics offer a self-care option in the facility that allows you to be in control of your treatment, but you still have the benefit of having trained staff available if you need their assistance. The dialysis facility schedules the dialysis treatment days and times according to the availability of openings in the facility. Every effort is made to schedule your treatment according to your specific needs. Some dialysis facilities offer an evening shift for those who work during the day.
Some clinics offer a self-care option in the facility that allows you to be in control of your treatment, but you still have the benefit of having trained staff available if you need their assistance. The dialysis facility schedules the dialysis treatment days and times according to the availability of openings in the facility. Every effort is made to schedule your treatment according to your specific needs. Some dialysis facilities offer an evening shift for those who work during the day.
Home Hemodialysis
 Home hemodialysis is a growing treatment option in which you, with or without a trained partner, can perform your hemodialysis treatments in the comfort of your own home. Home hemodialysis requires that you complete a training course. At first, you (and your partner, if you have one) will learn how to do the treatments in the clinic while working with a dialysis nurse. The length of training will vary for each patient, partner and dialysis facility. Training sessions (where you will complete your actual dialysis treatment while training) usually last four to five hours a day, three to four days per week for three to eight weeks. The education program will teach you all the necessary skills to dialyze safely at home. You will learn how to troubleshoot problems and how to properly manage emergencies. You will also be taught how to order your supplies. The equipment and supplies are delivered directly to you. The staff is available to answer your phone calls 24 hours a day. Home hemodialysis treatments allow for flexibility in the time of day you complete your treatment. For patients dialyzing at home without a partner, we offer remote monitoring of treatments via the Internet. Some types of home dialysis therapy can be done at night while you sleep. Even though you are completing all of your treatments at home, you will still need to meet monthly with your care team, either virtually (via telehealth) or in person, for blood work and for an assessment of your condition. Home hemodialysis is currently available in selected areas. If you are interested in home dialysis, you and your healthcare team can discuss the requirements, the responsibilities needed and locations where home dialysis is currently available.
Home hemodialysis is a growing treatment option in which you, with or without a trained partner, can perform your hemodialysis treatments in the comfort of your own home. Home hemodialysis requires that you complete a training course. At first, you (and your partner, if you have one) will learn how to do the treatments in the clinic while working with a dialysis nurse. The length of training will vary for each patient, partner and dialysis facility. Training sessions (where you will complete your actual dialysis treatment while training) usually last four to five hours a day, three to four days per week for three to eight weeks. The education program will teach you all the necessary skills to dialyze safely at home. You will learn how to troubleshoot problems and how to properly manage emergencies. You will also be taught how to order your supplies. The equipment and supplies are delivered directly to you. The staff is available to answer your phone calls 24 hours a day. Home hemodialysis treatments allow for flexibility in the time of day you complete your treatment. For patients dialyzing at home without a partner, we offer remote monitoring of treatments via the Internet. Some types of home dialysis therapy can be done at night while you sleep. Even though you are completing all of your treatments at home, you will still need to meet monthly with your care team, either virtually (via telehealth) or in person, for blood work and for an assessment of your condition. Home hemodialysis is currently available in selected areas. If you are interested in home dialysis, you and your healthcare team can discuss the requirements, the responsibilities needed and locations where home dialysis is currently available.
Nocturnal Hemodialysis
 Nocturnal dialysis is a treatment option for patients who choose to dialyze at night. Instead of dialyzing during the day, patients receive their treatment over a time period of about eight hours while they sleep. The treatment is usually prescribed three times a week. Because nocturnal dialysis is performed over a longer period of time and at a slower blood flow rate, patients do not usually experience complications such as low blood pressure and muscle cramping. The additional time on dialysis allows for better fluid and waste removal. Patients may even be able to decrease or discontinue some of their medications. Patients who have chosen nocturnal dialysis report that they feel healthier. This option is currently available in selected areas and may be available as a home hemodialysis option. If you are interested in this option, consult with your physician.
Nocturnal dialysis is a treatment option for patients who choose to dialyze at night. Instead of dialyzing during the day, patients receive their treatment over a time period of about eight hours while they sleep. The treatment is usually prescribed three times a week. Because nocturnal dialysis is performed over a longer period of time and at a slower blood flow rate, patients do not usually experience complications such as low blood pressure and muscle cramping. The additional time on dialysis allows for better fluid and waste removal. Patients may even be able to decrease or discontinue some of their medications. Patients who have chosen nocturnal dialysis report that they feel healthier. This option is currently available in selected areas and may be available as a home hemodialysis option. If you are interested in this option, consult with your physician.
What are the Possible Risks of Hemodialysis?
- Blood loss
- Decrease of blood pressure which can lead to the loss of consciousness and access complications
- Allergic reaction to the dialyzer material
- Air entering the bloodstream (air embolism)
- Muscle cramping
- Pain, bruising and swelling at the places where the needles are placed (infiltration)
- Clotting of the vascular access
- Infection